I spent a few days last week in a little city 115 miles south of Denver called Pueblo, where our newest health care center opened just a few months ago. Unfortunately, they’ve recently lost their only social worker, and I requested to travel on down to assist while the search for a replacement began. After all, everyone needs a little change from time to time, and if that happens to also include a free hotel and food for a few nights … well, then I figure why the heck not? However, what I found to be the most worthwhile part of the gig was the small caseload in Pueblo. The healthcare center there currently has only 50 clients since its opening. I normally carry a caseload of 70 by myself, this in addition to the caseloads of my 4 other co-workers in our Denver office, proves for a very busy office. Needless to say I was amazed at how much work I could accomplish at this new and seemingly bare facility.
One thing that I should probably mention is our health care centers not only house doctor’s offices and rehab gyms, but we also offer adult day centers. Here, seniors who are in need of socialization, or those who require daily supervision due to dementia, etc., can attend our center Mondays through Saturdays. As well, our philosophy of care strongly revolves around these client’s rights, and as such, those who are competent to do so are welcome to wander about the building as they wish. This creates a work environment that encompasses a lot of people seemingly just hanging around. I often receive ‘drop ins’ at my office throughout the day from clients who have questions, those just saying hello, or, more often than not, clients who simply want to talk. This is great, except that I am typically in the middle of WORK. I’ve found that some of my most beloved clients can tip toe on my last nerve when I’m taking a phone call and they are hovering in my doorway, or plopping down in a chair awaiting my attention. I am sure we’ve all experienced this kind of annoyance in the work place at some time.
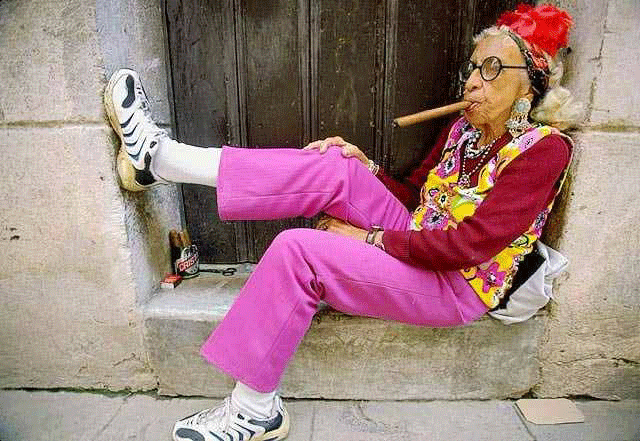
But, how can I honestly blame them… being that I work with seniors, the one thing they love to do is TALK. If you’ve ever spent any amount of time with a senior, you may know that they love conversation, to a point that breaks all social boundaries. I first learned this growing up around my grandfather, who, at the young age of 13, could corner me for over an hour talking about his time in the war. Much like grandpa, my clients don’t recognize normal social cues that indicate someone has lost interest or has checked out of the conversation. It’s not rare for me to spend hours at a person’s home during a routine home visit listening to their life time’s worth of experiences and stories, often not having even a chance to interrupt or mention that I’m late for my next appointment.
You may find it surprising that amongst the high rates of dementia and Alzheimer’s disease prevalent in the aging population, depression and anxiety rank right up there. As many clients on Aricept and Namenda (common drugs for memory loss) there are almost just as many on Lexapro and Celexa (common medications for depression and anxiety). When a new client joins our program, my assessment includes tests for both memory loss AND levels of depression. It’s a sad truth but when we’ve all retired, outlived many of our loved ones, and have suffered many debilitating physical losses, such as our eye sight and hearing, our world gets smaller. We end up seeing less of the world and it sees less of us. My belief, based on my experiences, is there is an overwhelming sense of loneliness encountered by the elderly. They have so much to share… and not enough people around willing to hear.
Prior to where I am at now, I worked as a volunteer coordinator for 2 years with a hospice agency. This was an incredibly rewarding job as I traveled throughout the city finding ways to infiltrate social and religious groups with the purpose of educating communities about the need for ‘friendly visitors’ among the senior population. Those home bound or living their life out in a nursing home are at the highest risk of isolation and depression. My current company’s volunteer program has developed much of its purpose around combating this issue of loneliness. We have between 100 and 200 volunteers, many of whom chose to give their time simply to spend an hour or so with a senior, providing companionship, and giving someone a little something to look forward to in an otherwise mundane existence. Just an hour. I’d encourage anyone looking for some way to give back to seek out a local hospice agency or other senior organization utilizing volunteers. My experience is that more often than not, the volunteer gains more than the people whom they are giving to.
So, on every Monday, Wednesday, and Friday when Jo Blow is scheduled to be at the adult day center, I better believe what he is looking forward to is talking to someone; anyone who will listen in fact… including that young, nice social worker at the end of the hallway. Frustration and annoyance aside, I find I must stop what I am doing and listen.
Saturday, September 18, 2010
Sunday, August 29, 2010
Geriatric terms, acronyms and definitions… words to know when working with or on behalf of seniors.
Dementia- A physical or organic syndrome (meaning not a mental illness nor psychological) which affects a person’s cognitive ability, i.e. memory and reasoning. Dementia is an umbrella diagnoses which envelops several different syndromes, the most notable being Alzheimer’s disease. Others include vascular dementia (often caused from a stroke), dementia with Lewy Bodies, Creutzfeldt-Jakob Disease, and the frontal temporal dementias including Picks disease and alcohol induced dementia (often seen in alcoholics). Dementia is also a standard and expected side effect of Huntington’s disease and Parkinson’s disease. Overall, dementia is a permanent and progressive disease in which a person loses the ability to remember what they had for breakfast, the names of their loved ones, how to get home and limits their reasoning skills. Medications do exist to treat dementia; Namenda and Aricept are two of the most used in my practice. Medication will not cure dementia, but is speculated to slow down its progression. Here, early detection and diagnoses is vital!
Geriatrician- Physician specializing in the elderly care. I highly recommend anyone over the age of 60 (55 depending on the policy) to begin seeing a geriatric physician. This would take the place of one’s primary care physician, which, can be hard for those who have had a lifelong relationship with their doctors. But, from my experience, issues experienced by those who are aging are so very specific, medication doses change, diagnoses suddenly stop being cured and instead become chronic and multiple, and with this is the issue of and counter indications becomes significant. Just like a child sees a pediatrician, as a senior I would encourage finding a geriatrician for my care.
ADLs- Activities of Daily Living- These include the very basic functions of living which are necessary to get by on a daily basis. Dressing, bathing, grooming, eating, ambulating (walking or ability to use a mobility device, i.e. wheel chair) are considered ADLs. When a person is no longer able to manage 1 or more of these functions without assistance, their ability to remain independent may become questioned. Often times a spouse or caregiver may be present to assist a person to complete all of their ADLs, thus enabling them to maintain. However, if there is no assistance available on a regular basis, a higher level of care may be needed, i.e. an assisted living facility or a nursing home.
Nursing home-Often referred to as a Skilled Nursing Facility (skilled, meaning medical) is a residence for people with constant medical need. This kind of facility has 24/hour medical staff consisting of nurses, certified nursing assistants (CNA), dieticians, physical therapists, occupational therapists, speech therapists, recreation therapists, medical directors (physicians who oversee the facility’s residents and daily procedures, etc.) as well as kitchen and housekeeping staff. Here, and ideally, everything a person needs is provided: room and board, medications, etc. A person must qualify, medically or otherwise, for placement at a nursing home. There are 2 components to which a person can be admitted: rehab or long term placement. A patient who’s just had surgery, i.e. a hip replacement, may need several weeks of rehab with a physical therapist, before they are able to successfully walk on their own again, manage pain, or complete ADLs independently. Thus, before going back home, they may spend several weeks at a nursing home and then return to their home. Payment for this is covered under Medicare Part A. As well, someone who is deemed unable to live independently ever again, like our advanced medical conditions and those with significant memory loss, can live permanently at a nursing home. Payment for permanent placement is typically covered either through private pay, some long term care insurances or Medicaid. Often times people must privately pay until their funds reach those of Medicaid criteria, and then Medicaid will kick in and pay for the remainder of the person’s stay.
Assisted living facility- A residence for those in need of some assistance on a daily basis. This is a non-skilled facility (meaning does not provide constant medical care) with 24/hour staff, which typically caters to seniors who are still able to manage most of their ADLs. Assisted living facilities provide meals and often times housekeeping and medication management. To be considered an assisted living facility (versus a group home) a nurse is usually required to be on staff for at least 8 hours a day. Other staff includes CNAs (certified nursing assistants), med techs (people trained to dispense medications), administrative staff, housekeeping, and maintenance and kitchen staff. In some situations, recreational staff is also available to provide activities. Some assisted living facilities cater to those with dementia and may be considered a “secured facility” meaning access into and out of the building is restricted without a key or code; this ensures the safety of those who may wander. Like nursing homes, an assisted living facilitie will ideally be all-inclusive providing everything a person needs to sustain, while usually offering a higher quality of life and independent status of living than that of a nursing home. For example these facilities are usually very aesthetically pleasing and people may still be functional enough to have their own cars to come and go and come as they wish. An assisted living facility will likely be a better option than a nursing home. Payment for assisted living is more often than not all private pay. Some long term care insurances may provide coverage and some (very few), and some facilities have limited rooms for those receiving Medicaid. The cost of this kind of facility is anywhere from $2,500 a month on up to $7,000-+$8,000 per month.
Medicaid- A program providing health insurance coverage for those who are considered low-income; children, pregnant women, parents of eligible children, people with disabilities and elderly needing nursing home care. Most residents of permanent stature at nursing home are covered by Medicaid (in a recent blog I noted that there are a million and a half people who currently live in nursing homes). Medicaid is reserved for those with financial and/or physical need. Its policies differ from state to state as Medicaid is jointly funded by states and the federal government. As well, Medicaid policy is changing constantly so it can be difficult to understand what Medicaid covers and what it doesn’t, and how it interacts with Medicare and private insurances.
Medicare- A social insurance program for those 65 and older and have paid into Medicare taxes for 10 years, or being a legal resident of the U.S. for 5 continuous years. As well, there are several stipulations in which a person under the age of 65 may qualify for Medicare, i.e. a person receiving dialysis, or those who’ve been receiving social security disability benefits and are diagnosed with qualifying medical conditions such as Lou Gerihg’s disease or ALS. Medicare has 4 parts to it which a person may be eligible for: Part A- Hospital coverage; Part B- medical coverage (i.e. the doctor’s office), Part C- Medicare Advantage, where a person has the choice to opt for their Medicare benefit to be provided by a private insurance; and Part D- prescription coverage. Most parts of Medicare include a deductible, copayment and/or premium of some sort. Medicare does NOT cover long term care, sitter services, or non-skilled in-home care.
Long Term Care Insurance-Insurance separate from that of health insurance, Medicaid or Medicare providing for the costs of long term care needs; potentially for that of nursing home costs, assisted living costs, sitter services, in home care, respite care, and other needs not typically covered but may be of significant cost to an individual. Coverage policies and rates differ from company to company.
PACE- Program for All-inclusive Care for the Elderly- a Medicaid/Medicare program for seniors in most state providing a holistic approach to healthcare. Criteria for this program include Medicaid financial eligibility and functional limitations that would make a person eligible for nursing home placement.
Private Sitter service- This is a non-skilled (meaning not medical) service that provides oversight to a person who is in need of a “babysitter,” for lack of a better term. Grandpa, grandma or a patient who is unable to remain at home alone, this service will provide a caregiver who is hired on an hourly basis; this caregiver can typically provide light housekeeping, cooking, take walks with clients, and provide stimulation through appropriate conversation and games (i.e. dominoes, cards, etc.). Sometimes families will also hire a sitter service to provide companionship to loved ones who may live alone and may be at risk for social isolation, like those at assisted living facilities, nursing homes, or perhaps someone who lives very far away. The draw back with a service like this is the hourly rates usually start at about $25 and for many people hiring someone to sit with mom, dad, aunt or grandma for a significant period of time can be a financial burden or outside of one’s resources.
MMSE- Mini Mental Status Exam; An assessment tool used to asses one’s cognitive functioning, i.e. how well is their memory working and how intact are their reasoning skills. The goal of this assessment is to screen for early stages of dementia and then track any decline from then on. The assessment is on a 30 question scale, 30 being a perfect score. Missing any more than 2 questions/tasks would indicate memory loss, often times associate to dementia. This assessment tool is not an exact science and has some limitations, but overall, it gives professionals an idea of where a patient is at mentally. I use this assessment on a daily basis at work. Per my agency’s policy, I re-assess every client every 6 months utilizing the MMSE in order to compare from year to year how they are doing. Ultimately, a person, professional or family member can be given a clear understanding of a person’s ability to safely remain independent (i.e. live alone) or how much assistance they should acquire on a daily basis, per the MMSE score. Things that may impact one’s MMSE score adversely and should be taken into consideration are mood and thought disorders, such as depression (someone suffering from depression may not score well, but not necessarily due to cognitive ability but rather due to the impacts of depression one’s thought process; here depression can be treated stopping any effects on their cognitive functioning).
SLUMS- St. Louis University Mental Status examination- this is an assessment tool much like the MMSE, but considered, among some professionals, to be a bit more sensitive to ascertaining memory loss, especially in individuals who have learned to compensate, thus, hiding any memory loss (often only possible in early stage dementia). Compensation is often observed in individuals with greater levels of education and economic standing. The SLUMS serves the same purpose as the MMSE but was developed later. Please see the MMSE definition for more detail.
GDS- Geriatric Depression Scale- An assessment tool used to identify depression in the elderly. The assessment asks 30 questions in which a patient will answer either ‘yes’ or ‘no’… Questions may include “Are you basically satisfied with your life?” and “Are you in good spirits most of the time?” A score greater than 9 is indicative of depressive symptoms.
APS- Adult Protective Services- A social service developed to protect senior adults, and sometimes disabled individuals, from abuse, neglect, and exploitation. APS is managed state to state differently by state health regulatory bodies. In Colorado, APS is managed by county. If abuse, neglect or exploitation is suspected, one can call and make a report to APS. Proof is not necessary, and the one reporting may remain anonymous if desired. APS has legal pull and rights to make decisions to protect at risk adults. However, seniors who are competent, those without significant memory loss, dementia, etc., who are making a choice to remain in an abusive, neglectful or exploitive situation, APS cannot force out of such a situation; not without request for help from that senior.
DNR- Do Not Resuscitate-A form which medical professionals facilitate for patients who do not wish to receive CPR (Cardio Pulmonary Resuscitation) or other life saving measures should their heart stop. Signing this form does not indicate that a person should not receive other normative treatments, such as antibiotics, dialysis, necessary surgeries, etc. As well, it’s important to note that CPR on a healthy 30 year old adult is VERY different than CPR on a senior adult. CPR on the elderly is not always a positive thing, even if it works and the person is revived; it often causes broken ribs and brings a person back in worse shape than before undergoing the process.
MDPOA- Medical Durable Power of Attorney- Known by different terms depending on which state a person is in (also known as MPOA-Medical Power of Attorney)- this is a completed form or paperwork in which a person (any person) may designate a person to make medical decisions for them in the event they are unable to do so; either because they are not conscious, or lack decision making capacity (indicated and documented by a physician). An MDPOA must be completed while a person is still competent to do so. After memory loss or dementia has progressed to moderate and especially advanced stages, a person may be deemed NOT competent to designate an agent, or person identified to make their medical decision for them. Again, depending on the state of residence, policies differ affecting whether an MDPOA requires witnesses or a notary to make it official (in Colorado neither are needed).
Sunday, August 22, 2010
Where are we all going?
I heard a story on NPR this week about a pastor from a church in Virginia, Kenneth Dupin, who is believed to be revolutionizing life for the elderly who are facing nursing home placement. He is the founder of the MEDCOTTAGE, or as the kids are calling it the “Granny Pod.” It’s basically a home on wheels (portable) with “advanced health monitoring equipment” that is intended to be placed in a family’s backyard where mom and dad or grandpa and/or grandma can live when they are no longer safe or able to remain in their own homes. Instead of facing institutional life, i.e. the nursing home, for a mere $2,000 a month, one can bring mom or dad home to live within arm’s length, and still offer some form of independence.
Albeit a great concept, Dupin has overlooked several factors that affect a person’s need for a nursing home. Like, how is mom, who is no longer ambulatory, supposed to get to the bathroom on her own during the day when daughter and son-in-law are at work from 8-5pm (sounds like a broken hip if you ask me). And, what about our beloved Alzheimer's patient who will (and I promise THEY WILL) wander out of that MEDCOTTAGE in a state of confusion while looking for ‘their home.’ Or, I love this one, how many seniors and their families can realistically afford $2000 a month for, essentially, rent? Not including monthly food, medicines, supplies, etc. The reality is such a concept may very well appeal to only a very small portion of the population; a portion who can, financially and physically, afford to have options. Of the “million and a half” seniors currently living in nursing homes across America, I doubt this concept will affect even 1% of them.
Let me tell you a little about why the typical nursing home resident goes into the nursing home: 1) their health is so severe that they require 24/hour nursing care simply to maintain; 2) their cognitive status is so lacking, due to some form of dementia, that they no longer recognize their family members, nor are they able to eat on their own, and they spend their days displaying obscene childlike behaviors or unsafe wandering; and 3) their family and loved ones live states away, or for whatever reason are not able or willing to take them in. I’d wage my bet that #3 is in fact the #1 reason any senior is institutionalized.
The sad fact is we live in a society (specifically white American society) that does not value caring for ‘our own.’ Rather than planning how we will care for our parents when they can no longer care for themselves, we PLAN on them going somewhere to live, where OTHER people will take care of them, where we don’t have to worry about it… or perhaps we avoid the subject all together. Because let’s face it, we simply don’t have the time or resources. Rather than handle the stress, the financial burden, or finding the time, we put them away!
But, did you know, in almost every other culture in the world, nursing homes are rare!... even a disgrace! Even in America, I find very few people of Hispanic, Asian, etc., dissents in a nursing home. And, during my master’s degree I had several classes with a girl from Russia, who was specializing in gerontology in order to take back what she learned to Russia, where nursing homes were just surfacing. She told me how in Russia, nursing homes were like 3rd world care, and no one wanted to send their loved ones to one because it was seen as shameful. It was a last resort, often for people without children. I’ll tell you from experience, most (and I say most to be pc, but I’d personally tell you ALL) nursing homes are basically 3rd world care. Compared to the care that one could receive from their own family, from people who actually know and love them… how could it truly compare?
In my practice, I make it a habit of comforting and relating to caregivers and family members who make the decision to place their loved ones in a nursing home. In fact, I am likely the one educating them about their option to do so. And, I especially empathize with the senior who is being placed, as this is not something any person at any time in their life hopes for. Although, I recognize this as the main reason we as a society can plan on life sucking after 70, I realize that society made its choice decades ago. When the family unit changed, i.e. divorce rates sky rocketed, fathers AND mothers began working full time, retirement age breached 73 years, etc., we also began to see the grandparent forgotten. And what decades ago did to produce such a mainstream phenomenon, I am not going to overturn by berating an overwhelmed caregiver for their choice to place their loved one at a facility. I respect this decision and do my best to ensure some quality of life from then on for that senior.
For myself, although my parents are only in their 40s, I am already thinking about how I and my siblings will plan to care for them as part of our individual families. I do hope that in some way, this will validate my parents’ lives as something meaningful… with something to look forward to beyond their retirement years… beyond the time when they can no longer give to society, or produce….. and give them continued hope… where one day they will die not alone in a stale room with unfamiliar things, but with those they love, and who love them… and where they are offered joy even at the end.
Otherwise… what are we all living for?
Albeit a great concept, Dupin has overlooked several factors that affect a person’s need for a nursing home. Like, how is mom, who is no longer ambulatory, supposed to get to the bathroom on her own during the day when daughter and son-in-law are at work from 8-5pm (sounds like a broken hip if you ask me). And, what about our beloved Alzheimer's patient who will (and I promise THEY WILL) wander out of that MEDCOTTAGE in a state of confusion while looking for ‘their home.’ Or, I love this one, how many seniors and their families can realistically afford $2000 a month for, essentially, rent? Not including monthly food, medicines, supplies, etc. The reality is such a concept may very well appeal to only a very small portion of the population; a portion who can, financially and physically, afford to have options. Of the “million and a half” seniors currently living in nursing homes across America, I doubt this concept will affect even 1% of them.
Let me tell you a little about why the typical nursing home resident goes into the nursing home: 1) their health is so severe that they require 24/hour nursing care simply to maintain; 2) their cognitive status is so lacking, due to some form of dementia, that they no longer recognize their family members, nor are they able to eat on their own, and they spend their days displaying obscene childlike behaviors or unsafe wandering; and 3) their family and loved ones live states away, or for whatever reason are not able or willing to take them in. I’d wage my bet that #3 is in fact the #1 reason any senior is institutionalized.
The sad fact is we live in a society (specifically white American society) that does not value caring for ‘our own.’ Rather than planning how we will care for our parents when they can no longer care for themselves, we PLAN on them going somewhere to live, where OTHER people will take care of them, where we don’t have to worry about it… or perhaps we avoid the subject all together. Because let’s face it, we simply don’t have the time or resources. Rather than handle the stress, the financial burden, or finding the time, we put them away!
But, did you know, in almost every other culture in the world, nursing homes are rare!... even a disgrace! Even in America, I find very few people of Hispanic, Asian, etc., dissents in a nursing home. And, during my master’s degree I had several classes with a girl from Russia, who was specializing in gerontology in order to take back what she learned to Russia, where nursing homes were just surfacing. She told me how in Russia, nursing homes were like 3rd world care, and no one wanted to send their loved ones to one because it was seen as shameful. It was a last resort, often for people without children. I’ll tell you from experience, most (and I say most to be pc, but I’d personally tell you ALL) nursing homes are basically 3rd world care. Compared to the care that one could receive from their own family, from people who actually know and love them… how could it truly compare?
In my practice, I make it a habit of comforting and relating to caregivers and family members who make the decision to place their loved ones in a nursing home. In fact, I am likely the one educating them about their option to do so. And, I especially empathize with the senior who is being placed, as this is not something any person at any time in their life hopes for. Although, I recognize this as the main reason we as a society can plan on life sucking after 70, I realize that society made its choice decades ago. When the family unit changed, i.e. divorce rates sky rocketed, fathers AND mothers began working full time, retirement age breached 73 years, etc., we also began to see the grandparent forgotten. And what decades ago did to produce such a mainstream phenomenon, I am not going to overturn by berating an overwhelmed caregiver for their choice to place their loved one at a facility. I respect this decision and do my best to ensure some quality of life from then on for that senior.
For myself, although my parents are only in their 40s, I am already thinking about how I and my siblings will plan to care for them as part of our individual families. I do hope that in some way, this will validate my parents’ lives as something meaningful… with something to look forward to beyond their retirement years… beyond the time when they can no longer give to society, or produce….. and give them continued hope… where one day they will die not alone in a stale room with unfamiliar things, but with those they love, and who love them… and where they are offered joy even at the end.
Otherwise… what are we all living for?
Friday, August 20, 2010
So, what's it all about?
I often feel I have the most interesting and eventful, as well as stressful, job in the world. Most of my days are spent talking with clients about their needs and comforting them in some way about the process of getting old. Things like, “who will take care of my wife when I have my hip replacement surgery?” or “what will I do when I can’t live at home by myself anymore?” and “I’ve lost my hearing aid.” I find myself saying things like “have you ever considered a long term care facility” and “yeah, no one ever warns you about getting old, do they?” This statement is always and immediately followed by “NO! They don’t!” Nonetheless, and deep down, I love what I do. Most people feel awkward around seniors, or perhaps don’t feel they know how to talk to them. Others don’t pay much attention at all. I find that these people are exceptional and unique personalities with decade’s worth of memories to tell and lessons to teach. Oh to be a fly on the wall in my office! Doting mothers, cursing veterans, and women with blue hair and dentures.
Subscribe to:
Posts (Atom)